Design and Analysis of Closed-Loop Medical Cyber-Physical Systems
Critical care involves the use of two common types of medical devices: monitoring devices, such as bedside monitors; and actuation devices, such as infusion pumps. Traditionally, caregivers need to collect information from the monitoring devices and manually adjust the settings of actuating devices. Patient safety may be compromised if a caregiver is diverted by an emergency and misses some important events. Physiological closed-loop interoperable systems have been proposed to solve this problem. In such a system, a controller is networked with sensors and actuators to continuously monitor the patient’s physiological states and automatically control the actuators within the safe operation region, thereby partially closing the loop. Caregivers will be alerted if the patient’s states become unstable.
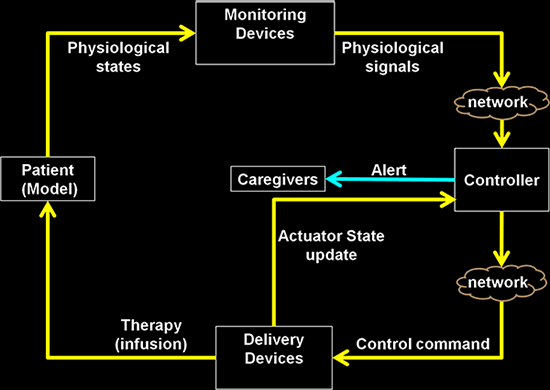 Patient safety is the primary concern in closed-loop MCPS. The complex interaction between the continuous time physiological dynamics of patients and the discrete, uncertain nature of networked control systems poses a major challenge on design and verification. We have developed a model-driven approach to prove the safety properties of MCPS. Our method combines simulation-based analysis of a detailed model of the system (including continuous-time patient dynamics) with model checking of an abstract timed-automata model. We have shown that crucial timing behavior is preserved across the two models, which ensures the conservativeness of the safety analysis. We have also proposed a system design that can guarantee open-loop safety under network failure. We have applied this approach to the development of a closed-loop Patient-Controlled Analgesia (PCA) system to prevent overmedication. We are currently working on extending the framework to more complicated clinical use cases such as closed-loop blood glucose regulation.
Patient safety is the primary concern in closed-loop MCPS. The complex interaction between the continuous time physiological dynamics of patients and the discrete, uncertain nature of networked control systems poses a major challenge on design and verification. We have developed a model-driven approach to prove the safety properties of MCPS. Our method combines simulation-based analysis of a detailed model of the system (including continuous-time patient dynamics) with model checking of an abstract timed-automata model. We have shown that crucial timing behavior is preserved across the two models, which ensures the conservativeness of the safety analysis. We have also proposed a system design that can guarantee open-loop safety under network failure. We have applied this approach to the development of a closed-loop Patient-Controlled Analgesia (PCA) system to prevent overmedication. We are currently working on extending the framework to more complicated clinical use cases such as closed-loop blood glucose regulation.
For more information on this and other cyber-physical systems projects, see the PRECISE Center.
Faculty
Students and Postdocs
- Hung Nguyen (PhD)
- Radoslav Ivanov (postdoc)
- Sooyong Jang (MS)
Funding
Sponsored by grants from NSF and NIH
Collaborators
University of Pennsylvania Healthcare System, Children’s Hospital of Philadelphia
